
“
Managing Parkinson’s disease symptoms is a critical aspect for patients and caregivers, involving a combination of medication, lifestyle adjustments, and supportive therapies. This approach helps improve mobility, mental health, and overall quality of life by addressing the progressive nature of this neurological disorder.1
1
”
Philosopher Friedrich Nietzsche believed that enduring illness can strengthen the human spirit, an idea echoed today as many Parkinson’s patients demonstrate resilience despite physical challenges. 1
Medication timing is crucial in managing Parkinson’s disease symptoms, as levodopa and dopamine agonists help regulate movement but must be carefully scheduled to reduce motor fluctuations. 2

Regular exercise improves muscle strength, balance, and coordination, significantly aiding symptom management by delaying progression and enhancing physical independence for Parkinson’s patients.
Speech therapy assists in overcoming common communication difficulties caused by Parkinson’s by improving vocal clarity and volume, which often decline as symptoms worsen. 3
A balanced diet rich in fiber, antioxidants, and omega-3 fatty acids supports brain health and can ease constipation, a frequent issue in Parkinson’s patients managing symptoms. 4
Occupational therapy helps adapt daily tasks to current abilities, promoting independence by teaching new techniques for dressing, eating, and household activities. 5
Deep brain stimulation surgery can reduce tremors and rigidity in some patients who no longer respond well to medication, offering an advanced management option. 6
Stress reduction techniques such as mindfulness and meditation help alleviate symptom severity by lowering anxiety, which often exacerbates motor and non-motor symptoms. 7
Sleep disorders frequently occur with Parkinson’s; managing these with good sleep hygiene and medical advice improves symptom control and daily functioning. 8
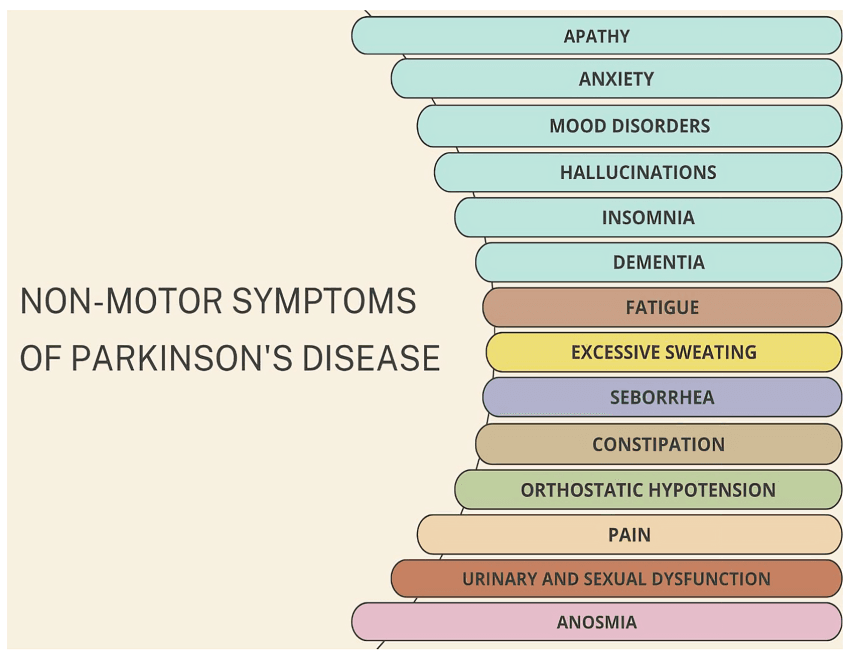
Non-motor symptoms like depression and anxiety require attention through counseling or medication, as mental health profoundly impacts symptom management success.
Vitamin D deficiency is common in Parkinson’s, and supplementing may support muscle function and reduce symptom severity when combined with other therapies. 9
Adaptive devices such as walking aids, special utensils, and button hooks improve autonomy by compensating for motor difficulties common in Parkinson’s. 10
Cognitive exercises and brain training activities help delay memory decline and improve concentration, which are often impaired in Parkinson’s disease progression. 11
Managing constipation with diet, hydration, and sometimes laxatives improves comfort and overall symptom control, as gastrointestinal issues are widespread in Parkinson’s. 12
Social support from family, friends, and support groups reduces feelings of isolation and depression, facilitating better coping with the chronic nature of Parkinson’s symptoms. 13
Tai Chi and yoga are gentle physical activities that enhance flexibility, balance, and mental calmness, assisting in the management of Parkinson’s symptoms. 14

Speech-language pathologists can also help manage swallowing difficulties, reducing the risk of aspiration pneumonia, a serious complication in advanced Parkinson’s cases.
Regular monitoring of blood pressure is important, as Parkinson’s patients often experience orthostatic hypotension, causing dizziness and increasing fall risk. 15
Occupational stress can exacerbate symptoms, so managing work-life balance and avoiding fatigue are practical steps to help control Parkinson’s disease effects. 16
Dr. Oliver Sacks stressed a multidisciplinary approach to Parkinson’s, noting that combining medication, therapy, and emotional support leads to the best outcomes for patients.17


