“
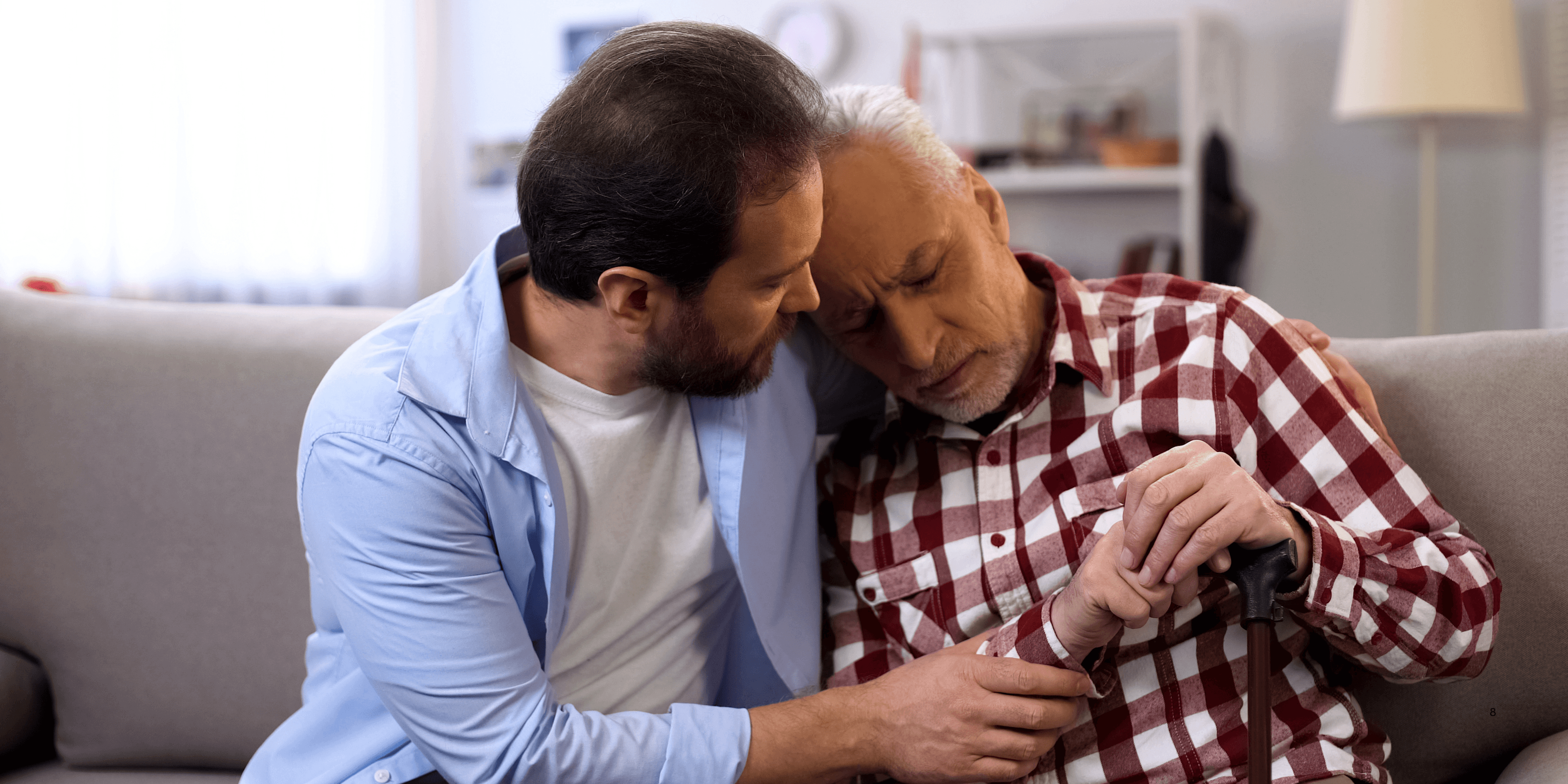
Managing pain & comfort in terminal illness is one of the most compassionate roles in healthcare. For older adults facing life-limiting conditions, comfort means more than medicine—it includes emotional presence, physical ease, and dignity. With the right balance of treatments and human connection, seniors can experience relief even in the most delicate stages of life.1
1
”
Terminal pain isn't just physical—it includes emotional, social, and spiritual discomfort. Effective care should treat the whole person, not just the illness, to provide truly meaningful relief. 1
Opioids like morphine remain essential in managing moderate to severe pain in terminal patients. When monitored correctly, they offer significant relief without shortening life or causing addiction concerns. 2

Complementary therapies such as massage, gentle acupuncture, and aromatherapy can reduce anxiety and ease chronic pain, especially when paired with medical treatments in hospice and palliative care settings.
Neuropathic pain, caused by nerve damage in cancer or chronic illness, may not respond to regular painkillers. Medications like gabapentin or antidepressants often help ease this type of pain effectively. 3
Breathlessness is a common and distressing symptom in terminal illness. Medications, oxygen therapy, and relaxation techniques like mindful breathing can ease this discomfort for older patients. 4
A warm, quiet environment with soft lighting can reduce physical tension and anxiety. Simple surroundings often promote comfort by minimizing stress and stimulating feelings of safety in elderly patients. 5
Terminally ill individuals may struggle with appetite and nausea. Small, frequent meals, ice chips, and anti-nausea medications can help them stay more comfortable and hydrated throughout the day. 6
Caregivers play a powerful role in managing comfort. Knowing when to reposition, provide a gentle massage, or just sit silently with a patient can make a profound difference in their day. 7

Palliative sedation is a last-resort option when suffering becomes uncontrollable. It gently induces sleep in dying patients, ensuring they feel no pain during their final hours.
Pressure sores are common in terminal illness due to immobility. Regular turning, special mattresses, and skin care routines reduce pain and keep the skin healthy and intact. 8
Constipation from painkillers or limited activity is a frequent concern. Gentle laxatives, hydration, and fiber-rich food—when possible—can make seniors feel more physically comfortable. 9
Some elderly patients experience terminal agitation or confusion. This may be soothed with gentle music, calming voices, or medication that relieves fear and brings mental peace. 10
A calm, well-trained hospice team—nurses, aides, social workers, and chaplains—ensures that no aspect of a patient's comfort is overlooked in their final journey. 11
Maintaining dignity means involving patients in decisions about their comfort plans, including where they wish to spend their final days—whether at home, in hospice, or in hospital. 12
Hydration may be limited in the final days, but frequent mouth care with ice chips or moist sponges helps maintain comfort and reduce feelings of dryness or thirst. 13

In some cases, unresolved grief can increase pain perception in dying individuals. Open conversations and emotional support allow healing while managing both body and spirit.
Repositioning the body every couple of hours relieves muscle tension and improves blood circulation—preventing discomfort from stiffness, pressure points, or bedsores in elderly patients. 14
A daily routine, even in terminal stages, can help provide a sense of normalcy and calm. Simple tasks like grooming or listening to the news can offer soothing familiarity. 15
Many seniors wish to be seen as whole persons, not just patients. Meaningful interactions, storytelling, and being addressed respectfully enhance emotional well-being until the end. 16
Physician Dr. Cicely Saunders, founder of modern hospice, believed that “pain has many forms, and so must comfort.” Her legacy reminds us to treat the person, not just the illness. 17


